There are an estimated 120 million people in the developing world with lymphatic filariasis, a painful disease that often leads to lymphedema. Once a parasitic filiarial worm called Brugia malayi is transmitted to a host through a mosquito’s saliva, they make their way to the lymphatics, where they grow and multiply. And when these worms have made themselves at home, there are few treatment options, because there are no lymphatic-localized therapies targeting the adult worms.
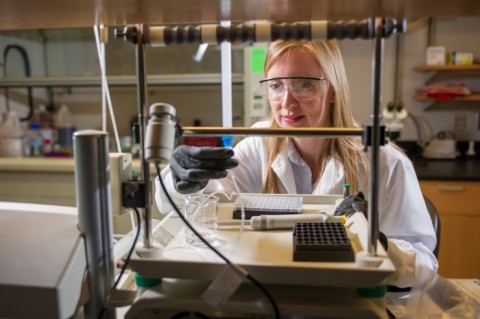
But research from the lab of Susan Thomas at the Parker H. Petit Institute for Bioengineering and Bioscience may offer new hope for the millions who already are infected and the billion people identified as at risk for infection.
“There are ways to prevent the transmission of the disease, but no way to treat people already affected by the adult worms,” says Thomas, assistant professor in the Woodruff School of Mechanical Engineering, whose research is detailed in a paper published in the journal Advanced Healthcare Materials.
“The major problem is, we can’t actually get drugs to the tissues to kill the worms,” says Thomas, also affiliated with the Wallace H. Coulter Department of Biomedical Engineering. “But we have designed nanoparticles with very strong lymphatic targeting activity.”
So Thomas and her team are using their targeted drug delivery scheme to treat lymphatic filariasis, encapsulating high amounts of nitric oxide (NO) into nanoparticles, which are injected into interstitial tissues, such as the skin, and then taken up, by lymphatics.
Results of the research suggest that therapeutic use of these NO-containing nanoparticles can eradicate Brugia malayi that reside within the lymphatic tissues, as well as for other deep tissue NO delivery applications.
Thomas's lymphedema-related research represents a longstanding collaboration with fellow Petit Institute faculty member J. Brandon Dixon – they trained together as post-docs, and Dixon is co-author of the research paper. Lead author of the paper, entitled “S-nitrosated polypropylene sulfide nanoparticles for thiol-dependent transnitrosation and toxicity against adult female filarial worms,” is Alex Schudel, a Ph.D. student in the Thomas lab. Timothy Kassis, a Ph.D. student in the Dixon lab, is also a co-author.
The targeted delivery technology at the heart of that research paper also has caught the attention of the Susan G. Komen Foundation, who awarded Thomas a three-year grant for $450,000 to study how the strategy might be used to deliver drugs to sentinel lymph nodes in breast cancer patients, a form of immunotherapy.
When cancer cells spread from a primary tumor in the breast, their first stop in the lymph nodes are typically the sentinel lymph nodes. Sentinel lymph nodes are the first lymph nodes to which cancer cells are most likely to spread from a primary tumor. Thomas has been exploring how targeted delivery of therapeutics could promote anti-tumor immunity and hinder tumor growth.
“Immunotherapy has the potential to treat tumors that we can’t actually see,” Thomas says. “But our immune system can see them. So this is a way of teaching our immune system to find the cancer and kill it, or prevent the disease occurrence. If we could teach our immune systems to kill, say, a breast tumor or breast cancer metastases or any other malignant tumor, that would be very beneficial in the long term.”
CONTACT:
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience
Jerry Grillo
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience
